“`html
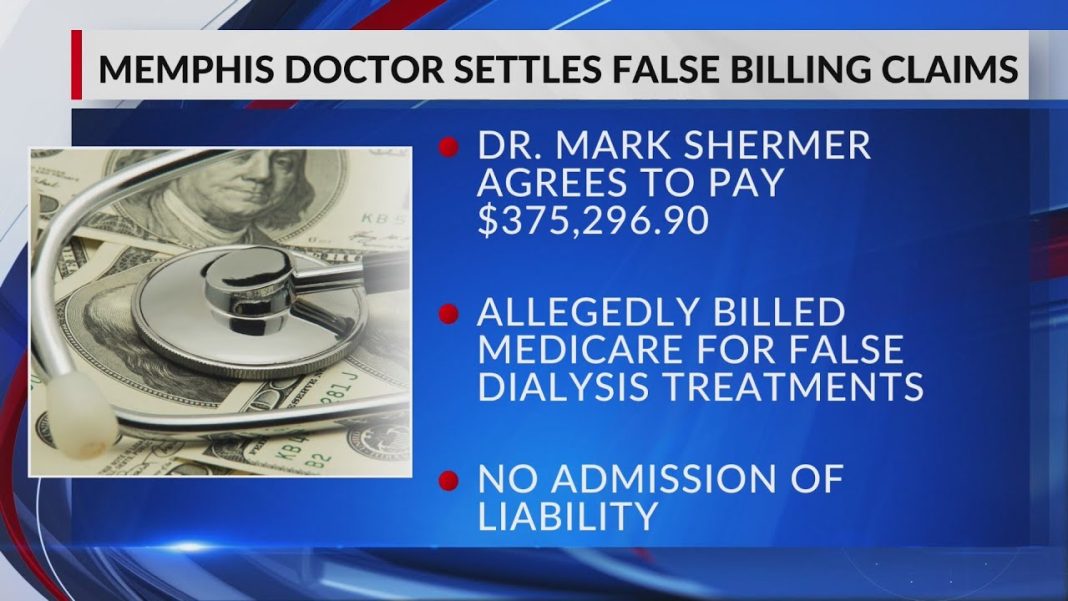
Memphis, TN – A local physician has reached a significant settlement in a fraud billing case, agreeing to pay $375,000 to resolve allegations of improper billing practices. The settlement comes amidst rising concerns over fraudulent activities in the healthcare sector, which have come under increasing scrutiny in recent years.
The doctor, whose name has not been disclosed, faced accusations of submitting false billing claims to Medicare and other insurers, inflating costs for services that were not provided or improperly billed. This case highlights the ongoing issue of billing fraud in the medical industry, where unethical practices have the potential to cost taxpayers millions of dollars.
According to federal prosecutors, the investigation revealed evidence that the doctor knowingly participated in a scheme to defraud health care programs. The decision to settle was made to avoid a lengthy legal battle, which could have resulted in more severe penalties or criminal charges.
The settlement is part of a broader initiative by the U.S. Department of Justice to combat healthcare fraud, which has seen a surge in cases. Authorities are emphasizing the importance of holding practitioners accountable to maintain integrity within the healthcare system and to safeguard taxpayer dollars.
In a statement, the doctor expressed regret for the actions that led to the settlement, emphasizing a commitment to ethical practices moving forward. Patients and the medical community alike were urged to remain vigilant against fraud and to report any suspicious activities.
This case serves as a reminder of the importance of vigilance in healthcare billing practices and the continued effort to protect patients and taxpayers from fraud.
“`